AMR Diagnostic Challenge Finalists
Five finalists will move on to the third and final phase of the AMR Diagnostic Challenge. The finalists were selected from a pool of 20 second-phase entries and will each receive $100,000 to further develop their prototypes. Step 2 finalists will submit their device prototypes by Jan. 3, 2020, for testing by two CLIA-certified independent laboratories. From the group of Step 2 finalists, up to three winners will share at least $19 million. Winners will be announced on July 31, 2020.
Project Title: Ultra-Rapid Infection Confirmation and Phenotypical AST by Microbe Mass Measurement
Principal Investigator: Ken Babcock
Institution: Affinity Biosensors
Executive Summary: The spread of antimicrobial resistance can be slowed by reducing the time needed to administer an effective, targeted antibiotic to infected patients. Our response to the AMR Challenge is a test that detects the presence of highly resistant strains of bacteria and also identifies the best targeted therapies in just a couple of hours, radically faster than the current standard of 2-3 days. The test employs a novel microfluidic sensor that weighs individual microbes at high throughput. Its rich data set rapidly detects bacterial growth and response to a panel of the most advanced antibiotics, and in key cases can do so even faster than the microbes themselves can multiply. The test targets blood stream infection and sepsis, acute urinary tract infection, and bacterial meningitis, maladies for which positive patient outcomes rely on rapid diagnostics. Notably, the test has been shown to successfully diagnose the most pernicious “superbugs,” i.e., those that are resistant to multiple advanced antibiotics and which are notoriously difficult to diagnose in rapid timeframes. Because it assesses growth phenotypically, the test will not be defeated as microbes evolve new resistance mechanisms, and it can be easily extended to additional sources of infection and to new antibiotics as they are developed. To ensure that the test will be readily adopted in the today’s clinical environment it has been automated, accommodates many samples, is easy to use, and is cost-effective.
Project Title: Patient-side, Disposable, Molecular PCR Diagnostic Device for Neisseria Gonorrhea and Drug Resistance Markers
Principal Investigator: Gary Schoolnik
Institution: Click Diagnostics, Inc.
Executive Summary: Click Diagnostics was founded with the mission to dramatically improve health outcomes by providing physicians with “patient-side” test results enabling immediate and accurate treatment. Through dramatic miniaturization, optimization, and cost reduction of laboratory polymerase chain reaction (PCR) technology, Click has created a fast, inexpensive, single-use (disposable) molecular diagnostic device. This device integrates and automates sample processing, PCR amplification, and amplicon detection into a simple, easy-to-use test. As the device does not require a separate instrument, it enables moving molecular testing from laboratories and large healthcare facilities to point-of-care locations, such as clinics, retail pharmacies, and eventually the home. Click’s first product for detecting the sexually transmitted infections N. gonorrhoeae, C. trachomatis and T. vaginalis is currently in a combined 510(k)/CLIA-waiver clinical study. In this project, Click is adding a Neisseria gonorrhoeae ciprofloxacin drug-susceptibility indication to this Sexual Health test. The CDC has classified Neisseria gonorrhoeae as an urgent threat since it is rapidly becoming resistant to antimicrobials. A point-of-care test, such as proposed here, integrating drug-susceptibility information with diagnostic testing will guide treatment decisions, improving patient outcomes through personalized treatment, extending the life of older antibiotics, and reducing the prescription of ineffective antibiotics.
Project Title: Fully automated pathogen ID and AST directly from whole blood and urine
Principal Investigator: Vincent G. Gau
Institution: GeneFluidics
Executive Summary: The emergence and rapid spread of resistant bacteria has become a serious public health concern worldwide. Delayed antimicrobial therapy significantly increases mortality in high-risk infections with a particularly strong association with septic shock. Therefore, antimicrobial agents are often injudiciously used without any evidence-based microbiological confirmation. Antibiotic consumption is strongly linked to the emergence and dissemination of antibiotic-resistant bacteria strains in several epidemiological studies. According to CDC’s recent publication, an estimated 30% of outpatient oral antibiotic prescriptions may have been inappropriate, and up to 70% of the “appropriate” prescriptions still require improvements in selection, dosage and duration to delay the development of antibiotic-resistant bacteria. The vast majority of antibiotic prescriptions are made by physicians outside the hospital setting without the use of a sophisticated diagnostic device. A compact and rapid pathogen identification (ID) and antimicrobial susceptibility testing (AST) can address both the unnecessary use and overuse of antibiotics, and therefore effectively reduce antibiotic microbial resistance. Our overall goal is to deliver a molecular diagnostic platform that is capable of rapid diagnosis of common bacterial infections in as short as 30 minutes and profiling their antibiotic resistance in as short as 90 minutes. Our product will lead to more rational use of antibiotics and will reduce the development and spread of multidrug-resistant pathogens. Our goal is to obtain the first FDA clearance of UtiMax, a rapid urinary tract infection ID/AST test currently in the pilot production stage, through a FDA de novo submission. A follow-up product line, BsiMax (with additional feature of lysis centrifugation), can process whole blood samples for bloodstream infections with a limit of detection (LOD) < 4 CFU/mL. Both UtiMax and BsiMax can be performed by our robotic liquid handling systems, with associated reagent kits and sensor chips. INTENDED USE – BsiMax (UtiMax) is a rapid diagnostics test to identify blood borne pathogens (uropathogens) directly from patients’ whole blood (fresh urine) samples. The BsiMax (UtiMax) ID/AST test can quantify the unique species-specific nucleic acid sequence associated with each target pathogen without using PCR and conduct antimicrobial susceptibility testing (AST) without a need of obtaining a clinical isolate or positive blood (urine) culture sample.
Project Title: Single Cell Biometric Analysis for Rapid ID/AST
Principal Investigator: Kyle Fieleke
Institution: Klaris Diagnostics
Executive Summary: Klaris is developing a single cell analysis platform that enables fast, targeted antibiotic treatment by delivering rapid pathogen identification (ID) and phenotypic antimicrobial susceptibility test (AST) results. We accomplish ID and AST using a new method that reduces system complexity, enables cost-effective testing, and permits testing directly from challenging non-sterile specimens. The Klaris platform utilizes phenotypic susceptibility testing methods, ensuring the clinical validity of current gold standard AST methods is maintained for rapid testing.
Conventional antibiotic susceptibility testing requires laboratory processing time that often exceeds 48 hours. As a result, clinicians must treat empirically, often utilizing broad spectrum antibiotics while they await culture results. This approach has triggered a cycle wherein empiric therapy regimens must periodically escalate to next-line antibiotics to account for increasing prevalence of resistance. Rapid ID/AST tests can help thwart this cycle by dramatically shortening the empiric treatment time window. Earlier therapeutic optimization will maintain patient outcomes while also helping to preserve a precious and limited public resource: the efficacy of our most potent antibiotics.
Project Title: Host Gene Expression to Classify Viral and Bacterial Infection Using Rapid Multiplex PCR
Principal Investigator: Ephraim Tsalik
Institution: Predigen, Inc.
Executive Summary: Inappropriately prescribed antibacterials for viral respiratory illness contribute to increased healthcare costs, unnecessary drug-related adverse effects, and drive antimicrobial resistance. The inability to rapidly and reliably distinguish bacterial from viral or non-infectious etiologies is a major impediment to appropriate antibiotic use. Currently available diagnostic strategies focus largely on pathogen detection although they are limited by poor sensitivity, long time-to-result, inability to distinguish infection from colonization, or restricted number of target pathogens. An alternative diagnostic strategy is to focus on the host’s response. The host (patient) responds to bacterial and viral causes of acute respiratory illness (ARI) in distinct and stereotypic ways. Based on that principle, we offer an innovative solution focusing on the patient’s response to infection. By combining machine learning analyses with system-wide gene expression measurements, we at Duke University and a recently formed spinout, Predigen Inc., have identified host response patterns that distinguish bacterial, viral, and non-infectious etiologies. Supported by the NIH-sponsored Antibacterial Resistance Leadership Group (ARLG), we embarked on a diagnostic development pathway called RADICAL (Rapid Diagnostics in Categorizing Acute Lung Infection), which has validated these host response signatures and supported a collaboration with BioFire Diagnostics. As a result, we have developed a 45-minute, sample-to-answer test that uses host gene expression to distinguish bacterial from viral infection.
AMR Diagnostic Challenge Semifinalists
Ten semifinalists were announced in the first phase of the AMR Diagnostic Challenge for their innovative concepts on point-of-need diagnostics tests to combat the emergence and spread of drug resistant bacteria. The semifinalists were selected from 74 submissions and each will receive $50,000 to develop their concepts into prototypes.
Project Title: Antimicrobial Resistance Rapid, Point-of-Need Diagnostic Test Challenge
Principal Investigator: Richard Anderson
Institution: Becton, Dickinson and Company, Franklin Lakes, New Jersey
Executive Summary: Becton, Dickinson and Company (BD) seeks to reduce the unnecessary use of antibiotics by guiding healthcare practitioners in differentiating between bacterial and viral infections within the time constraints of a single outpatient visit. Building on the public-health utility and broad commercial success of the BD Veritor™ platform, we are developing a novel digital immunoassay (DIA) that will measure a panel of circulating host immune biomarkers from a single blood-based sample. The test is intended to be an aid in the management of patients with symptoms of infection – such as upper respiratory infection – for which antibiotic misuse is a widespread problem. By providing objective diagnostic evidence that the patient’s immune system is fighting either a bacterial or a viral infection, the test will return an informative result without requiring a sample from the site of infection, and without the time or expense of diagnostic confirmation of numerous possible candidate pathogens. By employing the sample-in/result-out, one-button simplicity of the CLIA-waived BD Veritor system, the test can be deployed broadly at point-of-care settings without the need for trained personnel. And by returning a result rapidly (target of ten minutes) at the point of care, the test outcome will enable an actionable decision before the patient leaves the site.
Project Title: Breath volatile metabolites for the rapid identification of pneumonia etiology
Principal Investigator: Sophia Koo
Institution: Brigham and Women's Hospital, Boston, Massachusetts
Executive Summary: Community acquired pneumonia (CAP) is the fourth leading cause of death worldwide, with 430----450 million cases and 3----4 million deaths per year. In the United States alone, there are 4----5 million CAP cases, 1.1 million hospitalizations, and over 52,000 deaths annually, accounting for over $34 billion in direct health expenditures. Despite the high incidence of CAP, existing diagnostic tests for CAP are inadequate, identifying an underlying microbial pathogen in only 7----38% of cases. Even when a specific causal pathogen is identified, results often return long after it is necessary to make a clinical treatment decision. Because of the difficulty of identifying the microbial cause of pneumonia and the potentially severe consequences of not treating bacterial pneumonia promptly, clinicians often treat CAP empirically with antibiotics, even though a large proportion of these cases are viral in etiology. Unnecessary broad----spectrum antibiotic prescriptions per year, in turn, fuel the emergence and spread of resistant bacteria, including most of the urgent and serious threat level pathogens on the Center for Disease Control and Prevention’s list of urgent and antibiotic---resistant threats, on a population level. We propose a novel approach to CAP diagnosis based on distinct differences in the breath volatile metabolite profiles of patients with bacterial vs. viral pneumonia, using a rapid, portable gas chromatography--- differential mobility spectrometry (GC----DMS) Microanalyzer device at the point of care with parallel gold standard thermal desorption gas chromatography----tandem mass spectrometry (GC----MS/MS) in the laboratory to detect specific volatile metabolite signatures that (a) differentiate bacterial vs. viral CAP, and (b) identify certain common, specific causes of CAP, including Streptococcus pneumoniae. This rapid breath test for CAP would guide antimicrobial treatment decisions at the point of care, reducing antibiotic prescribing in patients who do not have bacterial pneumonia and slowing emergence of antimicrobial resistance on a population level.
Project Title: First Light's MultiPath platform
Principal Investigator: Don Straus
Institution: First Light Biosciences, Inc., Bedford, Massachusetts
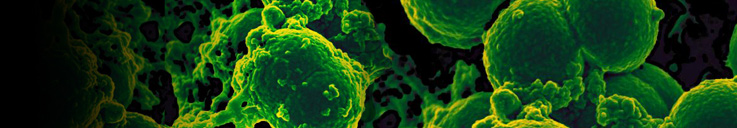
Executive Summary: First Light Biosciences is addressing two critical issues in healthcare: the rise in superbugs that are re-sistant to most antibiotics and the epidemic of hospital acquired infections. Today, a large fraction of life threatening infections seen in hospitals are caused by pathogens that are resistant to multiple anti-biotics. Effective treatment and cure requires rapid diagnostics to detect infections and select appropri-ate antibiotics for treatment. Unfortunately, no such tests exist today. We propose to develop tests based on First Light’s MultiPath technology that can rapidly and affordably detect a broad range of in-fections, accurately identify the infectious agents, and determine the appropriate antibiotic for treat-ment. The MultiPath platform consists of an automated benchtop analyzer that accommodates a broad menu of application-specific consumable cartridges. The MultiPath technology is quantitative. In only 15 min it detects infections and identifies pathogens including bacteria, fungi, viruses, toxins, human cells, and biomarkers. The technology can determine the correct antibiotic therapy in just 4 hours in contrast to the several days required by current methods. While as sensitive as high performance cen-tral laboratory tests, the MultiPath tests are as rapid and as easy-to-use as point-of-care tests and re-quire no sample preparation. The proprietary MultiPath technology achieves high sensitivity and quan-tification by using digital non-magnified imaging to count fluorescently labeled cellular and molecular targets. The MultiPath Platform eliminates labile enzymatic reagents, biochemical purification, and liq-uid handling (including wash steps), reducing complexity and cost while increasing throughput. We pro-pose to develop high-performance easy-to-use tests for important diagnostic applications for initial commercialization in the hospital setting. The platform and tests will also have commercial and medical advantages in outpatient settings. For Step 2, we plan to: (1) develop MultiPath assays for Clostridium difficile (C. difficile) diagnostics, multi-drug resistant Staphylococcus aureus (MRSA) surveillance, and urinary tract infection (UTI) diagnostics, (2) develop the MultiPath consumable cartridges for the three tests, (3) develop the benchtop automated MultiPath Analyzer, and (4) demonstrate the performance of the integrated MultiPath Analyzer and MultiPath Tests.
Project Title: Host gene expression to classify viral and bacterial infection using rapid multiplex PCR
Principal Investigator: Ephraim Tsalik
Institution: Duke University, Durham, North Carolina
Executive Summary: Inappropriately prescribed antibacterials for viral respiratory illness contribute to increased healthcare costs, unnecessary drug-related adverse effects, and drive antimicrobial resistance. The inability to rapidly and reliably distinguish bacterial from viral or non-infectious etiologies is a major impediment to appropriate antibiotic use. Pathogen detection strategies can be helpful but are limited by poor sensitivity, long time-to-result, inability to distinguish infection from colonization, or restricted number of target pathogens. Peptide biomarkers such as procalcitonin may also be helpful but are poorly sensitive and specific. Consequently, these approaches have not adequately addressed the antibacterial overuse problem. We therefore propose an innovative solution focusing on the patient’s response to infection. New scientific advances can now capture the entirety of the host response using system-wide molecular surveys (e.g., RNA, proteins, metabolites). We have developed analytical methods to define the stereotyped responses found within these highly complex and dense data. Applying these techniques to infection, we have shown the pattern of immune system response can distinguish bacterial, viral, and non-infectious etiologies. That response is most robustly detected in the patient’s gene expression profile, which is far more accurate than existing diagnostic tests. This strategy is only useful, however, if it can be measured rapidly, simply, and at the point-of-need. Supported by the Antibacterial Resistance Leadership Group, Duke University and BioFire Diagnostics now propose such a test. This simple-to-use, 1-hour test distinguishes bacterial infection, viral infection, or neither so as to guide the appropriate administration of antibacterials at the point-of-need.
Project Title: Minicare HNL: Point-of-care detection of bacterial infections to curb unnecessary use of antibiotics
Principal Investigator: Joe Frassica
Institution: Philips North America, Cambridge, Massachusetts
Executive Summary: Philips and the University of Pennsylvania (Penn) jointly propose development of a rapid, point of-care system to reliably rule out bacterial infection at primary care within minutes to avoid the unnecessary use of antibiotics. Between 80-90% of all antibiotics are prescribed in a primary care1 setting. Given the current misuse of antibiotics and related antimicrobial resistance, primary care settings can play an important role in reducing unnecessary antibiotic prescriptions2. Despite the benefits of using a point-of-care test to detect infectious disease biomarkers, adoption in primary care remains modest3. The reason for low adoption is that currently available biomarkers have low levels of clinical performance (i.e., sensitivity and specificity) and available tools require advanced skills to operate.
Philips is developing a unique approach to reliably detect bacterial infection at the point of care using a fast and easy-to-use test. The solution is designed to detect the biomarker Human
Neutrophil Lipocalin (HNL) on a diagnostic platform from a single drop of human blood. In 2015 the concept was successfully demonstrated with blood samples from patients with acute fever where in only minutes patients with a bacterial infection could clearly be distinguished from those without. To make this marker available in the primary care setting, Philips is working to realize the whole blood based assay onto its Minicare system. The CE-marked Minicare system is a platform for rapid blood testing, consisting of a point-of-care analyser and cartridges supporting different types of tests. Finalization of product development is estimated at 2.5 - 3 years. Penn will confirm performance of the biomarker using U.S. clinical samples in a separate study. Once test development is complete, Penn will serve as the clinical study site to validate and register the test and to perform a health technology assessment measuring its impact in reducing unnecessary prescription of antibiotics.
Project Title: Patient-side, disposable, molecular PCR diagnostic device for STI and Antimicrobial Resistance Detection
Principal Investigator: Gregory Loney
Institution: Click Diagnostics, Inc., San Jose. California
Executive Summary: Click Diagnostics was founded with the mission to dramatically improve health outcomes through innovative new diagnostic technology providing physicians with “patient-side” test results enabling immediate and accurate treatment. Through dramatic miniaturization, optimization, and cost reduction of laboratory polymerase chain reaction (PCR) technology, we have created a fast, inexpensive, easy-to-use, single-use (disposable) diagnostic device. Think “home pregnancy test,” but for nearly “any infectious disease.” Click has made patient-side testing for infectious diseases almost as simple as taking a patient’s blood pressure. We expect this to revolutionize health testing, moving molecular testing from laboratories and large healthcare facilities to doctors’ offices and clinics, and eventually the home. Because the Click device is fundamentally a PCR assay, products can be developed for most common infectious diseases such as sexually transmitted infections (STI), hospital-acquired infections (HAI), and respiratory infections. Our first product for detecting the STIs gonorrhea, chlamydia and trichomoniasis is scheduled for clinical trial in 2017. As part of the AMR challenge, we plan to add a test for drug resistant gonorrhea to this panel. The CDC identifies drug resistant gonorrhea as an urgent threat due to high levels of drug resistance and potential impact on public health.
Project Title: Rapid AMR Test using Spectral Platforms’ Technology
Principal Investigator: Ravi Kant Verma
Institution: Spectral Platforms, Inc., Monrovia, California
Executive Summary: We propose InSpector-01 (~ a rapid test for characterizing the presence/absence of pathogenic microorganisms in blood and urine samples) and InSpector-02 (~ a rapid test for characterizing the functional MIC minimum inhibitory concentration of a candidate antimicrobial required to suppress the growth of the causative pathogen, even prior to that pathogen being isolated and identified). InSpector-01 would be used to test blood and urine samples, both in the outpatient and in the inpatient setting, and would identify patients for whom antimicrobial therapy is inappropriate. Thus, InSpector-01 can reduce inappropriate antimicrobial use for the vast majority of patients who are currently treated with antimicrobials, but who are uninfected. InSpector-02 would be used to characterize blood samples in the inpatient setting for the functional MIC of the causative pathogen, so as to guide subsequent antimicrobial therapy (from the 2nd antimicrobial dose on). Both InSpector-01 and InSpector-02 offer unique capabilities ~ we are not aware of any other current/emerging methods that can identify patients for whom antimicrobial therapy is inappropriate (as InSpector-01 does) or current/emerging methods that can provide the functional MIC (as InSpector-02 does; other methods provide markers of specific resistance mechanisms). Both InSpector-01 and InSpector-02 are at an advanced stage of development, and are currently being field tested to develop a quality system necessary for distribution.
Project Title: Ultra-Rapid Phenotypical AST by Microbe Mass Measurement
Principal Investigator: Ken Babock
Institution: Affinity Biosensor, Santa Barbara, California
Executive Summary: The spread of antibiotic resistance can be slowed by reducing the time needed to administer an effective, targeted antibiotic to infected patients. Our response to the AMR Challenge is to produce a test that both confirms bacteremia caused by highly resistant strains, and provides a complete phenotypical antibiotic susceptibility test (AST) in a time that is radically shorter than today’s clinical standard. The test employs a microfluidic sensor that counts and weighs individual microbes at high throughput, and robustly measures bacterial culture growth at a speed limited only by the growth of the microbes themselves. It will provide clinically actionable information - confirming the presence of highly resistant bacteria and identifying the best targeted therapies - in hours or even minutes, vs. the current standard of 2-3 days. The initial targets will be CRE and ESBL-producing enterobacteriaceae, but the test will be extensible to all high-value bacterial targets and any desired antibiotics, and to a variety of bodily sources of infection (e.g., bacteremia/sepsis, spinal and pleural fluid, urinary tract, etc.) Because it assesses growth phenotypically, the test will not be defeated by evolving resistance mechanisms, and will provide an essential complement to resistance biomarkers and organism identification. The outcome will be the fastest possible sample-to result phenotypical susceptibility test, with the potential to migrate from a laboratory/in-patient setting to the doctor’s office.
Project Title: Transcriptional Profiling to Distinguish Bacterial and Viral Respiratory Infection
Principal Investigator: Ann Falsey
Institution: University of Rochester, Rochester, New York
Executive Summary: More accurate tests for microbiologic diagnosis of acute respiratory infections (ARI) are needed. Acute respiratory infections occur commonly throughout life, accounting for substantial morbidity and mortality in adults, and these infections are a leading cause of antibiotic overuse. Unnecessary antibiotic use is a major driver of the increase in antimicrobial resistance, which is considered to be one of the most urgent threats to global public health. In most cases of ARI, the precise microbial etiology is unknown and antibiotics are administered empirically in illness in both inpatient and outpatient settings. Although sensitive molecular diagnostics such as polymerase chain reaction (PCR) allow clinicians to rapidly and accurately diagnose a wide variety of respiratory viruses, their impact on patient management and antibiotic prescription has been modest primarily due to concern about bacterial co-infection. Sensitive and specific diagnostic tests for bacterial lung infection are currently lacking. Clinical parameters such as fever, purulent sputum, white blood cell count and radiographic patterns do not provide sufficient precision to reliably distinguish viral from bacterial infections. Thus, “ruling out” bacterial respiratory infection is extremely difficult, resulting in a default position of prescribing antibiotics to almost all patients hospitalized with respiratory infection and many outpatients as well. This practice results in significant antibiotic overuse, with resultant adverse effects and increased antimicrobial resistance. Recently, serum biomarkers such as procalcitonin have shown some promise as a supplement to clinical judgment in assessing patients with ARI but a need for more accurate tests remains. Gene expression profiling of whole blood represents a powerful new approach for analysis of the host response during infection. Preliminary studies indicate that viruses and bacteria may trigger specific host transcriptional patterns in blood, yielding unique “bio-signatures” that may discriminate viral from bacterial causes of infection. This approach can be used to supplement pathogen detection allowing clinicians to target antibiotic use for those patients that need treatment and thereby reducing unnecessary antibiotic use and resultant antimicrobial resistance. New rapid molecular diagnostics that incorporate detection of common respiratory viruses and bacteria combined with a limited number host genes discriminatory for bacterial and viral infection will be developed. The eventual goal is to simplify testing such that point of care ARI diagnostics can be employed in hospitals, emergency rooms, clinics and physicians’ offices for the maximal impact on patient care and antibiotic prescription.
Project Title: Yale's One Step, Rapid in vitro Diagnostic System
Principal Investigator: Ellen Foxman
Institution: Yale University, New Haven, Connecticut
Executive Summary: Every year, citizens of the United States experience more than one billion infections of the upper respiratory tract. Both viruses and bacteria can cause these illnesses but only bacteria are susceptible to antibiotics. However, we do not have a simple, rapid, comprehensive diagnostic test to distinguish between viral and bacterial upper respiratory infections. Lack of such tests contributes to the fact that outpatient visits for acute respiratory infection are the most common setting for inappropriate antibiotic prescriptions in the U.S, with about half of these prescriptions (~35 million prescriptions annually) not indicated1. Our recent findings indicate a way to develop a diagnostic test to rapidly distinguish between viral and bacterial causes of respiratory illness while the patient is in the doctor’s office. Unlike current tests, which detect the presence of specific viruses, this approach measures the response of the patient’s airway cells to the gmainfection to indicate whether the body is fighting a viral infection or a bacterial infection. This approach has two major advantages over current approaches: (1) many different viruses and bacteria can cause similar respiratory symptoms, but the only tests currently available are pathogen-specific. Therefore a single test can easily miss the organism causing the patient’s illness, and testing for large panels of pathogens is complex and can be prohibitively expensive; (2) unlike other proposed approaches to distinguish viral and bacterial infections based on the body’s response, our approach does not require a blood sample, but will work with a nose or throat swab. This test has tremendous potential to transform ingrained practices of prescribing antibiotics for non-bacterial illnesses by demonstrating the cause of infection to physician and patient during the initial healthcare encounter, and therefore will provide a powerful tool for promoting antimicrobial stewardship.